Medicaid recipients could lose health insurance
On March 31, continuous reenrollment for Medicaid recipients ended, meaning people who qualified for health care coverage through MO HealthNet kept their coverage for the past three years without having to renew annually.
MO HealthNet is Missouri’s Medicaid program that helps people with limited income and resources with their health care costs. People who are eligible for the program include pregnant women, children, someone responsible for a child under 19, someone with a disability or caring for a disabled family member, people aged 19 to 64, including parents and adults without children, and people 65 years or older.
Continuous enrollment in Medicaid began in January 2020 when the U.S. Department of Health and Human Services declared a public health emergency in response to COVID-19. As part of the CARES Act, signed into law on Dec. 29, 2022, Congress removed the continuous enrollment provision, and states were required to develop their own plans to again start checking the eligibility of all participants. Missouri’s Family Support Division (FSD), which is responsible for Medicaid applications and eligibility, started that process on April 1.
According to figures from the Missouri Department of Social Services, more than 1.4 million Missourians have health care coverage through MO HealthNet. The department estimates about 200,000 Missourians could lose their coverage either because they are no longer eligible, or they fail to complete the required paperwork to renew.
Maggie Schaffer, Case Management and Quality director at Bothwell Regional Health Center, said certain people are at a greater risk of losing their insurance coverage as a result of the return of annual renewals.
“People who have moved, people with disabilities, immigrants and people with limited English are at a higher risk of losing Medicaid coverage,” she said. “They may still be eligible but may not get the annual renewal letter or if they do, understand the process for renewal.”
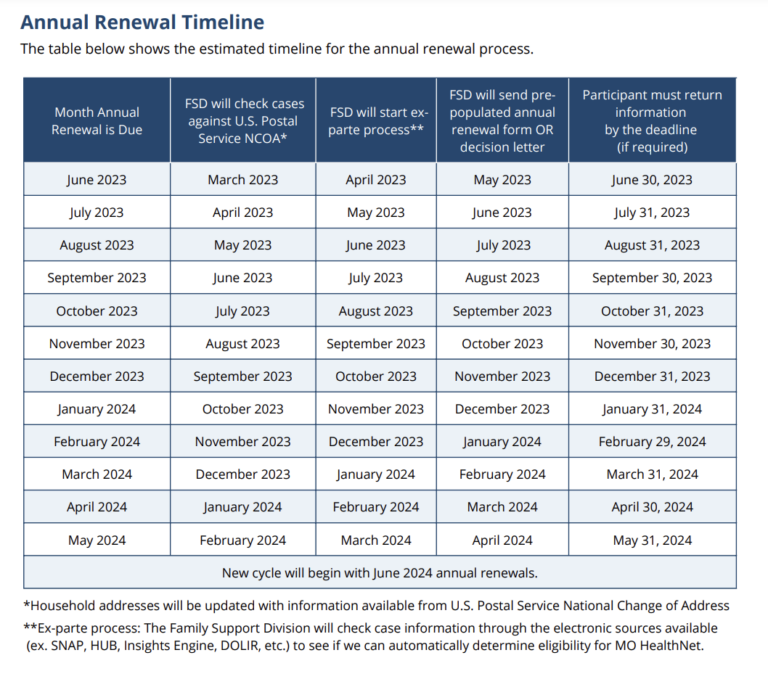
FSD has said participants’ renewal dates will typically be the anniversary month of when they originally enrolled in the program. The earliest renewal will be for a participant with a June renewal.
“Participants will receive a letter and they may need to submit more information to the state,” Schaffer said. “It’s really important that people make sure their address is correct with the state to ensure they receive the renewal notification so they don’t have a gap in coverage.”
To report changes to the Family Support Division, people can go online at mydss.mo.gov/renew, call 855-373-4636 or visit the Sedalia Family Support Division resource center at 808 Westwood.